Abstract
Background: Ibrutinib (ibr), a first-in-class, once-daily, covalent, Bruton's tyrosine kinase inhibitor, is approved in the US for treatment of patients (pts) with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), including pts with del(17p). The activity and safety of ibr in this early phase pivotal study was investigated in pts receiving first line ibr and pts with relapsed/refractory (R/R) CLL/SLL. We report data on the longest follow up available, up to 7 y, for pts receiving single-agent ibr.
Methods: Phase 1b/2 (PCYC-1102; NCT01105247) and extension study (PCYC-1103; NCT01109069) included pts receiving 420 mg (first line n=26; R/R n=67) or 840 mg QD ibr (first line n=5; R/R n=34) in the first line (≥65 y) or R/R (≥1 prior therapy) settings. Ibr was administered until disease progression (PD) or unacceptable toxicity. Efficacy was evaluated by investigator-assessed overall response rate (ORR, including partial response with lymphocytosis [PR-L]) using consensus criteria for CLL and SLL, duration of response (DOR; PR-L or better), progression free survival (PFS), and overall survival (OS). Responses were assessed for Döhner hierarchical subgroups. Median (95% CI) survival outcomes are reported. Adverse event (AE) monitoring was from first ibr dose until 30 days after the last dose; generally only grade ≥3 AEs and other significant AEs were collected on PCYC-1103.
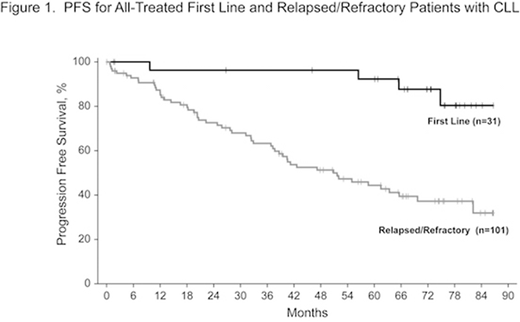
Results: Of 132 pts, 31 received first line ibr and 101 had R/R disease. As of the cutoff, 17 (55%) first line and 21 (21%) R/R pts continued ibr, with median (range) follow-up of 67 mo (0.7+, 87). Median (range) age for all pts was 68 y (37‒84); 43% of pts were ≥70 y (first line, 74%; R/R, 34%). Baseline genomic characteristics have been reported and included many high-risk features such as complex karyotype (first line, 13%; R/R, 37%) and unmutated IGHV (first line, 48%; R/R, 78%). R/R pts received a median (range) of 4 prior therapies (1‒12). ORR was 89% for all pts (complete response [CR], 15%), with similar rates in first line (87% [CR, 32%]) and R/R pts (89% [CR, 10%]). Median DOR was not reached (NR; 95% CI: not estimable [NE], NE) for first line and was 57 mo (38, 80) for R/R pts. Median PFS was NR (95% CI: NE, NE) for first line and was 51 mo (37, 70) for R/R pts (Fig 1); estimated 7 y PFS rates were 80% and 32%, respectively. Median OS was NR in first line (95% CI: 80, NE) or R/R pts (63, NE), with estimated 7 y OS rates of 75% and 52%, respectively. Median OS for pts with PD within 1, 3, and 5 y of treatment initiation was 13 (95% CI: 1, 25), 28 (17, 54), and 57 mo (28, NE), respectively. In R/R pts, median PFS was 26 mo (95% CI: 18, 37) in 34 pts with del(17p), 51 mo (31, 62) in 28 pts with del(11q), 82 mo (7, NE) in 5 pts with trisomy 12, and NR (63, NE) in 13 pts with del(13q). Median PFS was NR (95% CI: 40, NE) in 16 R/R pts with no abovementioned cytogenetic abnormalities. Among R/R pts, median PFS trended longer for 27 pts with 1‒2 prior lines of therapy (66 [95% CI: 37, NE]) versus 14 pts with 3 (59 [22, NE]) or 60 pts with ≥4 prior lines of therapy (39 [26, 51]). The primary reason for treatment discontinuation in first line pts was AEs (23%), whereas in R/R CLL it was PD (35%). Most common AEs (≥2 pts) leading to discontinuation were diarrhea, subdural hematoma, and sepsis (n=2 each). Grade ≥3 AEs were reported in 74% of first line and 89% of R/R pts, and serious AEs were reported in 61% of first line and 76% of R/R pts. Hypertension (first line, 32%; R/R, 26%) and pneumonia (first line, 10%; R/R, 27%) were among the most common grade ≥3 treatment-emergent AEs. A similar proportion of first line (10%) and R/R pts (9%) experienced major hemorrhage. Grade ≥3 atrial fibrillation (first line, 6%; R/R, 10%) and infection (first line, 23%; R/R, 55%) were more common in R/R pts. In all pts, grade ≥3 treatment-emergent AEs were highest during the first year of treatment and subsequently declined.
Conclusions: With up to 7 y of follow-up, sustained activity of single-agent ibr was observed with first line ibr and for R/R pts with CLL/SLL, including those with high risk genomic factors. Responses were durable, with stable or improved CR rates, and sustained PFS and OS rates (estimated 7 y rates: 80% and 75% for first line pts and 32% and 52% in the highly pretreated R/R population, respectively). In R/R CLL, ibr administration in earlier lines of therapy resulted in improved PFS outcomes, with longer PFS after 1‒2 versus ≥3 prior lines of therapy. Ibr was acceptably tolerated, and most grade ≥3 AEs declined over time.
Furman:Loxo Oncology: Consultancy; Genentech: Consultancy; Verastem: Consultancy; Sunesis: Consultancy; Incyte: Consultancy, Other: DSMB; TG Therapeutics: Consultancy; Janssen: Consultancy; Gilead: Consultancy; AbbVie: Consultancy; Acerta: Consultancy, Research Funding; Pharmacyclics LLC, an AbbVie Company: Consultancy. Coutre:Beigene: Consultancy; Gilead: Research Funding; Pharmacyclics LLC, an AbbVie Company: Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Celgene: Research Funding; AbbVie: Consultancy, Research Funding. Flinn:Janssen: Research Funding; Kite: Research Funding; Novartis: Research Funding; Agios: Research Funding; Merck: Research Funding; Calithera: Research Funding; Curis: Research Funding; Portola: Research Funding; Gilead: Research Funding; Genentech: Research Funding; Pfizer: Research Funding; Seattle Genetics: Research Funding; Verastem: Consultancy, Research Funding; Incyte: Research Funding; Trillium: Research Funding; Pharmacyclics: Research Funding; Takeda: Research Funding; TG Therapeutics: Research Funding; ArQule: Research Funding; Forty Seven: Research Funding; Constellation: Research Funding; Celgene: Research Funding; Infinity: Research Funding; BeiGene: Research Funding; Verastem: Research Funding; Forma: Research Funding. Blum:Morphosys: Research Funding; Novartis: Research Funding; Seattle Genetics: Research Funding; Celgene: Research Funding. Sharman:Pharmacyclics, an AbbVie Company: Consultancy, Research Funding; Acerta: Consultancy, Research Funding. Wierda:Genentech: Research Funding; AbbVie, Inc: Research Funding. Luan:Pharmacyclics, LLC, an AbbVie Company: Employment; AbbVie: Equity Ownership. Liu:AbbVie: Equity Ownership; Pharmacyclics, an AbbVie Company: Employment, Other: TRAVEL, ACCOMMODATIONS, EXPENSES. Dean:CTI BioPharma Corp.: Employment, Equity Ownership; Pharmacyclics LLC, an AbbVie Company: Employment; AbbVie: Equity Ownership. O'Brien:Gilead: Consultancy, Research Funding; Regeneron: Research Funding; Sunesis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Celgene: Consultancy; Astellas: Consultancy; Aptose Biosciences Inc.: Consultancy; Abbvie: Consultancy; Pharmacyclics: Consultancy, Research Funding; Acerta: Research Funding; Janssen: Consultancy; TG Therapeutics: Consultancy, Research Funding; Amgen: Consultancy; Alexion: Consultancy; GlaxoSmithKline: Consultancy; Kite Pharma: Research Funding; Vaniam Group LLC: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal